In today’s digital age, enhancing communication and engagement with your patients is more important than ever. One of the most effective tools at your disposal is the patient portal. This online platform can transform how you interact with patients, making communication more efficient and fostering a deeper level of engagement. Let’s explore how you can utilize patient portals … [Read more...] about Using patient portals to enhance communication and engagement
Health care reform
The Office Manager’s Part in Facilitating Video Calls Between Providers and Patients
Video calls have become a vital part of healthcare delivery, offering patients the convenience of seeing their doctor without leaving home. As a medical office manager, you play a critical role in ensuring that video consultations run smoothly, benefiting both patients and providers. Here's a comprehensive guide to help you facilitate seamless video calls in your … [Read more...] about The Office Manager’s Part in Facilitating Video Calls Between Providers and Patients
Better patient communication for better care and engagement
Effective patient communication is at the heart of a successful medical practice. It's not just about delivering medical care; it's also about creating a meaningful and lasting relationship with your patients. In today's digital age, the landscape of communication has expanded, offering numerous channels to connect with patients. From appointment reminders to follow-up care … [Read more...] about Better patient communication for better care and engagement
How to navigate compliance and regulatory updates
In the ever-evolving healthcare industry, medical office managers play a pivotal role in ensuring that their practices not only adhere to current healthcare regulations but also anticipate and adapt to forthcoming changes. Compliance and regulatory updates are not merely legal obligations but cornerstones of patient safety, quality care, and operational success. In this … [Read more...] about How to navigate compliance and regulatory updates
Strategies to stay updated with healthcare regulations
One of your paramount responsibilities is ensuring that your practice adheres to the myriad of healthcare regulations that govern the industry. Compliance isn't just a legal obligation; it's a cornerstone of patient safety, operational efficiency, and the overall credibility of your practice. Here's why staying updated with healthcare regulations is crucial and how you can … [Read more...] about Strategies to stay updated with healthcare regulations
HIPAA compliance quiz for medical office employees
Instructions: This quiz is designed to test your knowledge of HIPAA (Health Insurance Portability and Accountability Act) requirements and regulations. Please select the best answer for each question. Choose only one answer unless otherwise specified. Good luck! Question 1: What does HIPAA stand for? a) Health Insurance Policy and Administration Act b) Health Information … [Read more...] about HIPAA compliance quiz for medical office employees
Physician Fee Schedule Updates for 2025 hit Telehealth, Payment Policies, Rates and Quality
The 2025 Medicare Physician Fee Schedule (PFS) introduces several key updates that impact payment policies, rates, and quality provisions: Payment Rates: There are refinements to codes for services addressing social determinants of health, with a focus on expanding the use of billing codes for social risk assessments and care coordination. Complexity add-on payments for … [Read more...] about Physician Fee Schedule Updates for 2025 hit Telehealth, Payment Policies, Rates and Quality
HIPAA compliance checklist
Having a complete HIPAA compliance program is important to your organization. Run through this HIPAA compliance checklist to see if you have your foundation of HIPAA compliance in place and easily retrievable. HIPAA Policies and Procedures HIPAA privacy policies, procedures, and forms HIPAA security policies, procedures, and forms HIPAA Breach Notification policy and … [Read more...] about HIPAA compliance checklist
Integrating telemedicine into your practice
The healthcare landscape is evolving, and telemedicine has emerged as a transformative tool for medical practices to expand their reach, improve patient access, and provide high-quality care remotely. Integrating telemedicine services into your practice requires careful planning and execution, considering aspects like technology, staff training, patient communication, and … [Read more...] about Integrating telemedicine into your practice
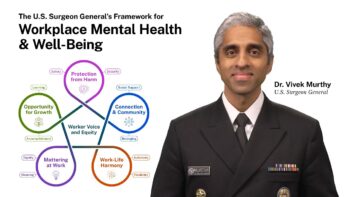
Five essentials to support employee mental health and well-being
Events of the last four years have changed the nature of work for many and the relationship that some workers have with their jobs. The Surgeon General’s Framework for Mental Health & Well-Being in the Workplace outlines the foundational role that workplaces should play in promoting the health and well-being of workers and communities. With more than 160 million … [Read more...] about Five essentials to support employee mental health and well-being