By Steve M. Cohen bio I usually focus more on the serious sides of personnel management, the kind of issues that can close down a business or organization if mishandled. "Getting organized" might not sound like one of those issues, but I've witnessed cases where disorganization was clearly a factor in success and failure. Especially in environments like those faced … [Read more...] about Get organized or suffer
Technology
Will video kill the medical office visit?
In a world of ever-advancing technology, "the doctor will see you now" has taken on new meaning. Video conferencing allows patients to consult with physicians without leaving home. Physicians, meanwhile, have the advantage of treating routine illnesses without involving practice staff or tying up examination rooms and other facilities. For both parties, it seems to be a … [Read more...] about Will video kill the medical office visit?
Important guidelines for your medical practice website
When your medical office establishes a website, be sure to set some boundaries and limits for individuals using that website, and give careful attention to the individuals referenced at the site. To set boundaries for individuals using the site, you should have a terms-of-use policy available on the website which includes disclaimers about the purpose of the site and what … [Read more...] about Important guidelines for your medical practice website
Health care providers optimistic but losing confidence in ACA according to study
While more than three-quarters of health care providers express optimism about the future of U.S. health care overall, support for the Affordable Care Act (ACA) has lessened according to a new study by Mortenson, one of the leading health care contractors in the United States. The number of health care providers who feel positive about the ACA has fallen significantly in … [Read more...] about Health care providers optimistic but losing confidence in ACA according to study
Do your patients need medication reminders?
When prescribing medication, physicians provide patients with dosage information. Pharmacies also provide this information when filling prescriptions. Nevertheless, patients often have a difficult time remembering what and how much medication to take when. The situation can be especially problematic when a patient takes multiple prescription drugs. With this mind, your … [Read more...] about Do your patients need medication reminders?
Secrecy in the age of social media: six ways to keep sensitive practice information offline
You can be sure that most of your employees are active on social media. For younger ones, in fact, using Facebook, Instagram, and Twitter are as natural as breathing. According to James Pooley, author of "Secrets: Managing Information Assets in the Age of Cyberespionage," social media and the sharing culture it has sparked are very real threats to organizations. "The … [Read more...] about Secrecy in the age of social media: six ways to keep sensitive practice information offline
Try this “win-win” solution to stop personal internet use by staff
Manager Beth C. Pharr of North East Orthopaedics in Tupelo, MS, relies on a basic management practice when she presents any new policy. "I make it a win-win situation," she says. "I tell staff 'this why it's necessary, and this is how it benefits you.'" Such was the case when Pharr set a policy to solve a problem common to almost every office – personal internet use. To … [Read more...] about Try this “win-win” solution to stop personal internet use by staff
Three electronic conveniences also help with EHR requirements
A Columbus, MS, pediatrics practice has added three electronic items that not only provide convenience for patients but give the office EHR meaningful use credit. First is online bill paying. That's provided through the office's billing service, says Sabrina McDow, CEO of Children's Health Center of Columbus. The invoices give a website for the online payments, but because the … [Read more...] about Three electronic conveniences also help with EHR requirements
Use rating sites to improve your medical practice
Many people rely on rating sites for hotels, restaurants, and other vacation and leisure activities. But consulting a rating site before making an appointment with a physician, and allowing that site to influence a health care decision? It's more common than you might think. A survey conducted by the University of Michigan finds among people using physician-rating sites, 35 … [Read more...] about Use rating sites to improve your medical practice
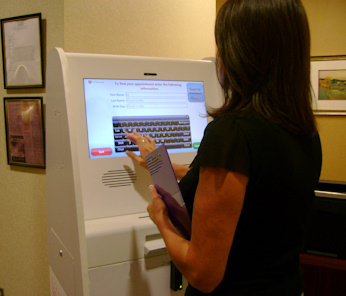
Patient self-scheduling offers advantages for busy medical practices
Demand for greater convenience will change the way patients schedule appointments in the near future. Approximately two-in-three patients (64 percent) are expected to book medical appointments online by the end of 2019, according to research conducted by Accenture, a global management consulting, technology services, and outsourcing company. "Just as consumers use online … [Read more...] about Patient self-scheduling offers advantages for busy medical practices